Why Treatment for Stress Incontinence in Females is Vital
By Leah Fulker, PT, DPT, PCES, MTY-1
In my role as a pelvic floor physical therapist, I've encountered a multitude of women who have shared to following experiences:
- Initially downplaying their bladder leaks, only to realize their severity over time.
- Facing a significant decline in confidence and a strain on relationships due to incontinence.
- Feeling restricted in daily activities, as to avoid uncomfortable bladder accidents, further impacting social outings and relationships.
Questions arise about clothing choices, incontinence pads, and the availability of bathrooms, creating a burden that prompts the inevitable question, “Why didn't I seek help sooner?”
Sometimes, I will see patients who seek help right away, for issues like how to stop urine leakage when coughing, when treatment for stress incontinence in females can be more manageable. However, more often I see many who have endured bladder leaks for several years before seeking help.
In this article, my aim is to empower women to seek treatment and solutions for bladder leaks. Despite its challenges, bladder leaks are not normal and there's hope for freedom from this burden.
Understanding the Potential Cause of Stress Incontinence
Bladder leaks, one type medically known as stress urinary incontinence (SUI), occurs when the muscles and tissues supporting the bladder and urethra become weakened or damaged, leading to involuntary urine leakage during activities that put pressure on the bladder, such as coughing, sneezing, laughing, or exercising.
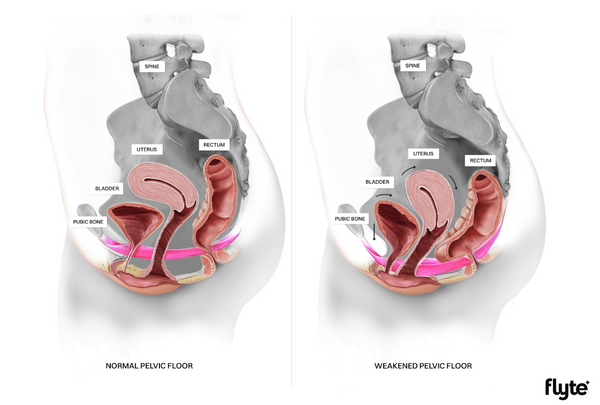
This form of bladder leakage in women is often associated with pregnancy and childbirth, when the pelvic floor muscles undergo significant strain, leading to urinary symptoms. The hormonal fluctuations accompanying menopause can further negatively impact pelvic floor function, amplifying the risk of SUI.
Take the FREE Incontinence Quiz
Stress Incontinence: The Domino Effect
Bladder leaks, even seemingly minor ones, can take a significant toll on women's lives, impacting their social interactions, daily activities, self-assurance, and even their intimate relationships.
I've encountered women in my clinic who, due to embarrassment and fear of urinary leakage, have withdrawn from sexual intimacy and social engagements, resigning themselves to isolating at home. This withdrawal continues a cycle of pelvic floor and general muscle weakness, emotional distress, and physical discomfort—a cycle we urgently need to break.
Compounding these personal experiences are findings from medical studies, which paint a stark picture of the consequences of women's incontinence:
- Women who develop SUI during pregnancy are 579% more likely to have stress urinary incontinence (SUI) 1-year postpartum. (1)
- Women with incontinence have a 41% urinary tract infection (UTI) rate vs 9% without incontinence. (2)
- Urinary incontinence is a strong indicator of functional problems later in life. A 2017 study on female nursing home residents in Switzerland found over 50% of the women had urinary incontinence upon admission and more than 80% needed help with their activities of daily living. (3)
These insights highlight the need to address bladder leaks comprehensively, not only to ease immediate symptoms but also to safeguard long-term well-being.
Stress Incontinence Treatment for Women
As a healthcare provider, I deeply empathize with the countless women who suffer silently from bladder leaks and stress incontinence, often delaying seeking help for various reasons. Many perceive it as a normal part of aging or motherhood, perhaps influenced by the experiences of their mothers or friends who also endure similar challenges. Additionally, feelings of embarrassment or the belief that their leaks aren't severe enough often deter women from discussing their symptoms with healthcare professionals.
However, it's essential to recognize that ignoring stress incontinence won't make it disappear, and in fact, urinary incontinence typically worsens over time if left untreated. Fortunately, there are numerous female bladder solutions to get control:
Seek Professional Help
Seeking professional guidance is crucial in addressing bladder leaks. Schedule an appointment with your healthcare provider or consider consulting a pelvic floor physical therapist. These experts can assess your condition, provide personalized advice, and recommend tailored treatment options. We offer a complimentary Ask a Pelvic Physical Therapist service to help with education and guidance.
Perform Pelvic Floor Exercises
Pelvic floor exercises, like Kegels, play a pivotal role in strengthening the muscles that support the bladder and pelvic organs to help stop stress incontinence. To ensure optimal results, visit our article, How to do Kegels correctly and enhance results for comprehensive guidance on mastering this beneficial exercise.
Not sure if Kegels are right for you? Check out our article To Kegel or not to Kegel or schedule a call with our Ask a Pelvic Floor Physical Therapist.
Try At-Home Treatments like Flyte
Revolutionizing urinary incontinence treatment, Flyte offers a convenient, at-home, and clinically proven solution for women seeking relief from bladder leaks. Say goodbye to the limitations imposed by stress incontinence and embrace the freedom to live life on your terms, all from the comfort of your home in only 5 minutes a day.
Avoid Bladder Irritants
Certain fluids can exacerbate bladder irritability and contribute to urinary incontinence. Managing these bladder irritants is essential for minimizing leaks and maintaining bladder health. Discover practical tips in our article, Sip smarter by learning to manage these 4 bladder irritants.
Take Back Control
Living with stress incontinence and relying on pads shouldn't define our daily existence. Just because we may have had kids and we are all getting older, doesn’t mean we have to live with the burden of buying pads or being too afraid to remain active anymore!
These risk factors have been proven to lead us down a road of consequences that extend beyond physical discomfort, leading to isolation, depression, and inactivity. It's time to say no more to limitations and stigma. Let's prioritize pelvic health and seek the care we deserve.
1. Gill, B., Moore, C. and Damaser, M., 2010. Postpartum stress urinary incontinence: lessons from animal models. Expert Review of Obstetrics & Gynecology, 5(5), pp.567-580.
2. Raz, R., 2011. Urinary Tract Infection in Postmenopausal Women. Korean Journal of Urology, 52(12), pp.801-808.
3. Schumpf, L., Theill, N., Scheiner, D., Fink, D., Riese, F. and Betschart, C., 2017. Urinary incontinence and its association with functional physical and cognitive health among female nursing home residents in Switzerland. BMC Geriatrics, 17(1).











